What is the aim of this review?
Coronavirus (COVID-19) is a respiratory infectious disease that has spread throughout the world. Healthcare workers treating patients with COVID-19 are at risk of infecting themselves and others by breathing in droplets from infected patients and touching contaminated surfaces. Governments and organisations publish infection prevention and control (IPC) guidelines to reduce transmission of infections. IPC guidelines cover using personal protective equipment (PPE) like masks, gloves, and gowns; separating patients with respiratory infections; and stricter cleaning routines. However, how much healthcare workers follow this guidance varies.
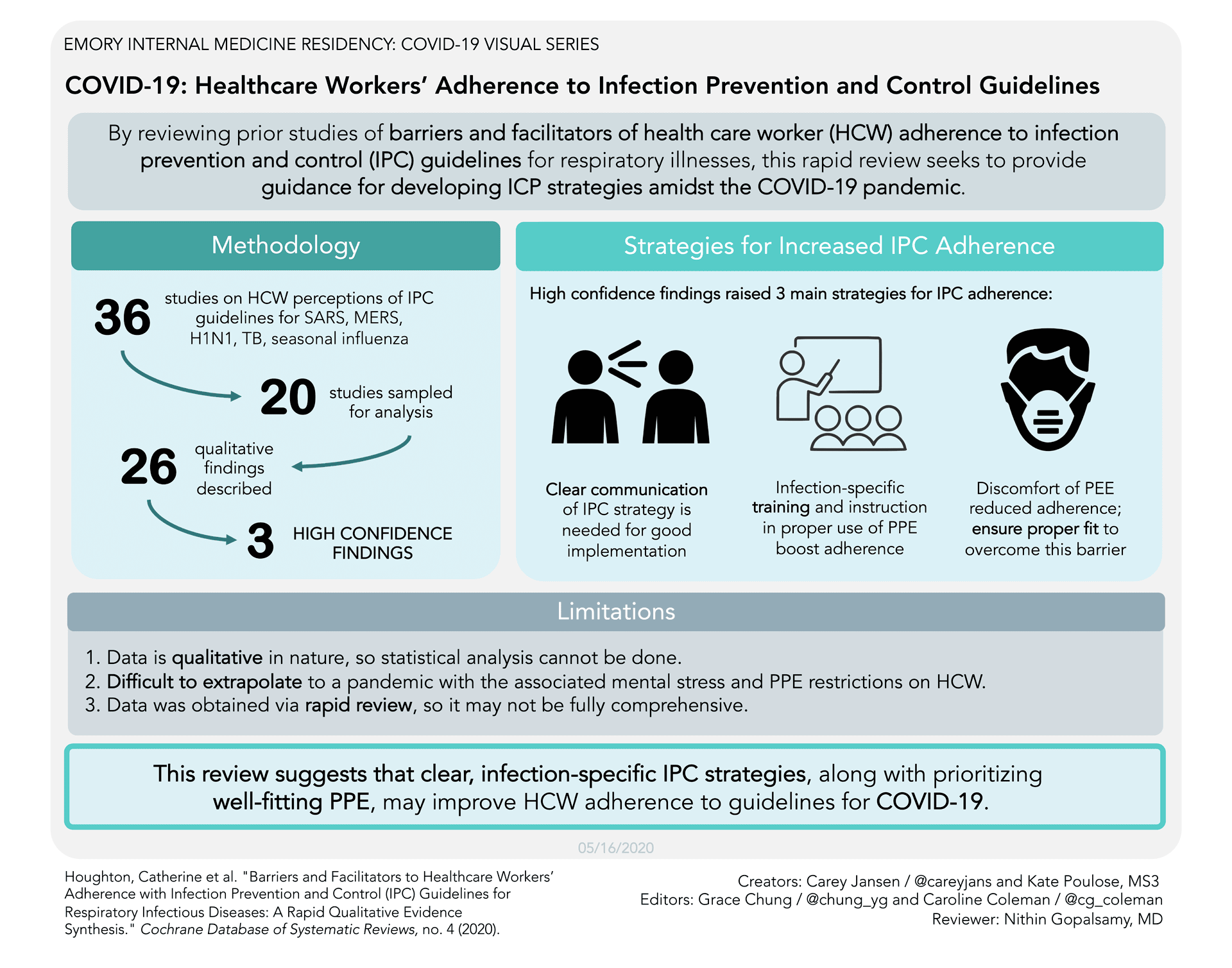
The aim of this Cochrane review of qualitative research (“qualitative evidence synthesis”) was to explore what influences whether healthcare workers follow infection prevention and control (IPC) guidelines for respiratory infectious diseases. To answer this question, we analysed 20 qualitative studies of healthcare workers' views and experiences of IPC guidelines.
Key messages
Healthcare workers point to several factors that influence their ability and willingness to follow IPC guidelines when managing respiratory infectious diseases. These include factors linked to the guideline content and how it is communicated, support from managers, workplace culture, training, physical space, access to and trust in personal protective equipment (PPE), and a desire to deliver good patient care. The review also highlights the importance of including all healthcare facilities staff when implementing guidelines.
What was studied in this review?
We searched for studies that examined healthcare workers’ views and experiences towards IPC guidelines – particularly for respiratory diseases that start suddenly, like COVID-19. Guidelines could be local, national, or international, for any healthcare setting. We included studies of any healthcare worker who looked after patients in any healthcare setting. We searched for studies published from 2002 onwards to cover the 2003 severe acute respiratory syndrome (SARS) outbreak onwards.
What are the main findings of this review?
We analysed 20 studies. Ten studies were from Asia, four each from Africa and North and Central America, and two from Australia. The studies explored the views and experiences of nurses, doctors and other healthcare workers when dealing with SARS, H1N1 (‘swine flu’), Middle East respiratory syndrome (MERS), tuberculosis or seasonal influenza. Most healthcare workers worked in hospitals.
Our review pointed to several factors that influenced healthcare workers’ adherence to IPC guidelines. We judged the following findings to be well supported or very well supported (moderate to high confidence) by the studies we found.
Healthcare workers were unsure whether to follow local guidelines if they differed from national or international guidance. They struggled to follow long or unclear guidelines, especially if their advice was impractical or kept changing. Use of PPE and additional cleaning meant that following IPC guidelines increased workload and fatigue. Healthcare workers’ responses to IPC guidelines were influenced by the support they received from management and their workplace culture.
Healthcare workers emphasised the importance of clear communication about IPC guidelines. But healthcare workers pointed to a lack of training about the infection itself and about how to use PPE. They thought it was a problem when training was not compulsory and believed all staff, including cleaners, porters, kitchen and other support staff, should be included in IPC training.
Insufficient space to isolate patients, and lack of anterooms, showers and easy access to handwashing facilities was a problem. Practical measures, such as minimising overcrowding, fast-tracking infected patients and restricting visitors were important for reducing infection.
Lack of, and poor-quality, PPE was a serious concern for healthcare workers and managers. Supplies need to be adjusted as infection outbreaks continue. Healthcare workers found PPE uncomfortable to use and some found PPE made patients feel isolated and frightened.
Healthcare workers believed that they followed IPC guidance more closely when they saw its value, for example, reducing the risk of infecting themselves and their families, or protecting their patients.
Many factors affect healthcare workers’ willingness and ability to follow IPC guidelines. Our review includes a set of questions drawn from our findings to help healthcare providers plan, implement, or manage IPC strategies to help their workers follow IPC guidelines.
How up-to-date is this review?
This review includes studies published up to 26 March 2020.
Healthcare workers point to several factors that influence their ability and willingness to follow IPC guidelines when managing respiratory infectious diseases. These include factors tied to the guideline itself and how it is communicated, support from managers, workplace culture, training, physical space, access to and trust in personal protective equipment, and a desire to deliver good patient care. The review also highlights the importance of including all facility staff, including support staff, when implementing IPC guidelines.
This review is one of a series of rapid reviews that Cochrane contributors have prepared to inform the 2020 COVID-19 pandemic.
When new respiratory infectious diseases become widespread, such as during the COVID-19 pandemic, healthcare workers’ adherence to infection prevention and control (IPC) guidelines becomes even more important. Strategies in these guidelines include the use of personal protective equipment (PPE) such as masks, face shields, gloves and gowns; the separation of patients with respiratory infections from others; and stricter cleaning routines. These strategies can be difficult and time-consuming to adhere to in practice. Authorities and healthcare facilities therefore need to consider how best to support healthcare workers to implement them.
To identify barriers and facilitators to healthcare workers’ adherence to IPC guidelines for respiratory infectious diseases.
We searched OVID MEDLINE on 26 March 2020. As we searched only one database due to time constraints, we also undertook a rigorous and comprehensive scoping exercise and search of the reference lists of key papers. We did not apply any date limit or language limits.
We included qualitative and mixed-methods studies (with an identifiable qualitative component) that focused on the experiences and perceptions of healthcare workers towards factors that impact on their ability to adhere to IPC guidelines for respiratory infectious diseases. We included studies of any type of healthcare worker with responsibility for patient care. We included studies that focused on IPC guidelines (local, national or international) for respiratory infectious diseases in any healthcare setting. These selection criteria were framed by an understanding of the needs of health workers during the COVID-19 pandemic.
Four review authors independently assessed the titles, abstracts and full texts identified by the search. We used a prespecified sampling frame to sample from the eligible studies, aiming to capture diverse respiratory infectious disease types, geographical spread and data-rich studies. We extracted data using a data extraction form designed for this synthesis. We assessed methodological limitations using an adapted version of the Critical Skills Appraisal Programme (CASP) tool. We used a ‘best fit framework approach’ to analyse and synthesise the evidence. This provided upfront analytical categories, with scope for further thematic analysis. We used the GRADE-CERQual (Confidence in the Evidence from Reviews of Qualitative research) approach to assess our confidence in each finding. We examined each review finding to identify factors that may influence intervention implementation and developed implications for practice.
We found 36 relevant studies and sampled 20 of these studies for our analysis. Ten of these studies were from Asia, four from Africa, four from Central and North America and two from Australia. The studies explored the views and experiences of nurses, doctors and other healthcare workers when dealing with severe acute respiratory syndrome (SARS), H1N1, MERS (Middle East respiratory syndrome), tuberculosis (TB), or seasonal influenza. Most of these healthcare workers worked in hospitals; others worked in primary and community care settings.
The review points to several barriers and facilitators that influenced healthcare workers’ ability to adhere to IPC guidelines. The following factors are based on findings assessed as of moderate to high confidence.
Healthcare workers felt unsure as to how to adhere to local guidelines when they were lengthy and ambiguous or did not reflect national or international guidelines. They could feel overwhelmed because local guidelines were constantly changing. They also described how IPC strategies led to increased workloads and fatigue, for instance because they had to use PPE and take on additional cleaning. Healthcare workers described how their responses to IPC guidelines were influenced by the level of support they felt that they received from their management team.
Clear communication about IPC guidelines was seen as vital. But healthcare workers pointed to a lack of training about the infection itself and about how to use PPE. They also thought it was a problem when training was not mandatory.
Sufficient space to isolate patients was also seen as vital. A lack of isolation rooms, anterooms and shower facilities was identified as a problem. Other important practical measures described by healthcare workers included minimising overcrowding, fast-tracking infected patients, restricting visitors, and providing easy access to handwashing facilities.
A lack of PPE, and provision of equipment that was of poor quality, was a serious concern for healthcare workers and managers. They also pointed to the need to adjust the volume of supplies as infection outbreaks continued.
Healthcare workers believed that they followed IPC guidance more closely when they saw its value. Some healthcare workers felt motivated to follow the guidance because of fear of infecting themselves or their families, or because they felt responsible for their patients. Some healthcare workers found it difficult to use masks and other equipment when it made patients feel isolated, frightened or stigmatised. Healthcare workers also found masks and other equipment uncomfortable to use. The workplace culture could also influence whether healthcare workers followed IPC guidelines or not.
Across many of the findings, healthcare workers pointed to the importance of including all staff, including cleaning staff, porters, kitchen staff and other support staff when implementing IPC guidelines.